[This article is part of our Transgender Breast Health Series.]
Hormones are a hot topic in both transgender circles and breast cancer research. Since breast cancer is so tied to gender, educators in our breast health education programs are often asked how breast cancer risk changes for the transgender community. We’ve previously discussed sex reassignment surgery. Here’s what you need to know about transgender hormone therapy and its impact on breast cancer.
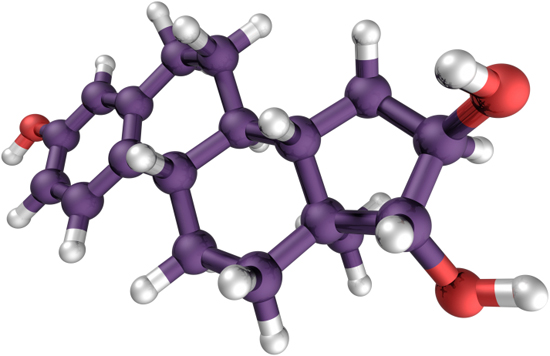
Estrogen & Testosterone
Estrogen, the principle female sex hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs., is naturally found in the bodies of both men and women, though in larger quantities in women. Eighty percent of all breast cancers are hormone-receptor-positive, which grow according to the body’s supply of estrogenA female sex hormone that is primarily produced by the ovaries. Its primary function is to regulate the menstrual cycle and assist in the production of secondary sex characteristics such as breasts. It may even play a role in the production of cancer cells in the breast tissue.. We don’t know exactly how estrogenA female sex hormone that is primarily produced by the ovaries. Its primary function is to regulate the menstrual cycle and assist in the production of secondary sex characteristics such as breasts. It may even play a role in the production of cancer cells in the breast tissue. helps breast cancer to grow, but we know that it’s related, and much of our current preventative measures and breast cancer treatments involve reducing the estrogenA female sex hormone that is primarily produced by the ovaries. Its primary function is to regulate the menstrual cycle and assist in the production of secondary sex characteristics such as breasts. It may even play a role in the production of cancer cells in the breast tissue. levels in our bodies. Knowing this, it’s easy to understand the concern from the transgender community—estrogen is also the main hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs. taken by men transitioning to female.
Estrogen isn’t the only hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs. though. There are also concerns about testosterone, the principle male sex hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs., and main hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs. taken by transgender men. Excess testosterone (a type of androgenAny male hormone. The most commonly known is testosterone. Sometimes used in the treatment of metastatic breast cancer. hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs.) can be converted by the body into estrogenA female sex hormone that is primarily produced by the ovaries. Its primary function is to regulate the menstrual cycle and assist in the production of secondary sex characteristics such as breasts. It may even play a role in the production of cancer cells in the breast tissue., where it can then help breast cancer to grow.
The Effects of Hormone Therapy
Most researchers agree that both transgender men and women who have never taken hormones have the same breast cancer risk levels as persons assigned their same sex at birth. But for those that have taken hormones, preliminary studies show that hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs. therapy may have an effect on breast cancer risk levels.
The largest study to examine breast cancer and transgender hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs. therapy is a 2019 Dutch cohort study that followed over 2000 trans women and 1000 trans men. The study found that, compared to the reference non-transgender male group, the study participants had a higher rate of breast cancer, but it was still lower than the non-transgender female reference group. Study participants did, however, become diagnosed at an earlier age than the non-transgender female reference group.
The problem is that while we know hormones do effect breast cancer and risk levels, we understand very little about exactly how the complicated MTF (male-to-female) and FTM (female-to-male) hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs. therapy drugs effect these risk levels. Transgender hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs. therapy is still an emerging field and there is still a lot of research to do.
Melanie McDermet, M.S., a geneticInherited characteristics. counselor at Winthrop University Hospital, also adds, “The advice we would have for a trans individual considering hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs. therapy, would be exactly the same advice for a postmenopausal woman considering hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs. replacement therapy. Everyone should obtain a thorough family medical history. Patients should discuss any cancer history in their family, especially any known geneticInherited characteristics. mutations, with their doctor. They may make a referral for a consultation with a certified geneticInherited characteristics. counselor. The geneticInherited characteristics. counselor may encourage certain individuals to undergo genetic testing to better assess cancer risks. At this time, there is no recommendation on how to proceed with hormoneA chemical substance produced in the body that controls and regulates the activity of certain cells or organs. therapy when a trans individual is found to have a harmful geneticInherited characteristics. mutation. But awareness of this mutation should stimulate additional discussion of the increased risk.”
Your Risk Factors
With so little clear research on breast cancer risks as it related to transgender hormones it’s easy to be overwhelmed and a little confused about how to proceed. But there’s a lot we do know for sure that will improve your health:
- Find a trans-friendly primary care doctor that you trust. More healthcare providers are receiving transgender care and sensitivity training than ever before. It is becoming increasingly easier to find a doctor that understands your unique care needs with an office setting that respects privacy.
- Reduce your controllable breast cancer risk factors—smoking, alcohol, obesity, and lack of exercise. Regardless of your gender identity, everyone can benefit from this.
- Get an annual mammogram if you are over 40 and you are a transgender woman who has taken hormones or have other risk factorsAnything that increases or decreases a person’s chance of developing a disease., of if you are a transgender man who has not had chest surgery.
- Do a monthly breast self-exam regardless of your gender identity.
- If you are taking hormones, take them as prescribed, and make sure they are from a trusted source.
No matter your gender identity, your breast health is vital. With a better understanding of breast cancer risk factorsAnything that increases or decreases a person’s chance of developing a disease. and how they relate to hormone therapy, you, with the help of your doctor should feel empowered to make positive healthcare decisions.